Review of Classic Research Paper
Respiratory Syncytial Virus (RSV) and Human Metapneumovirus (HMPV) are two closely related pathogens within the Pneumoviridae family that are frequently confused in cases of pediatric acute respiratory infection. While their clinical presentations overlap, prospective surveillance data (2016–2020) from 7 US children’s hospitals—involving 8,605 patients—reveal critical differences in their high-risk populations, disease severity, and clinical management. This study employed an active, prospective design with systematic nasopharyngeal swab collection and testing for 8 respiratory viruses, providing the first large-scale, real-world comparison for pediatricians. By analyzing hospitalization rates, ICU admissions, mechanical ventilation use, and prolonged hospital stays (≥3 days), it establishes a crucial pre-intervention epidemiological baseline for the era of new RSV immunizations (e.g., maternal vaccines, long-acting monoclonal antibodies) and creates a framework for future HMPV vaccine development.
Key Finding 1: Distinct High-Risk Profiles
-RSV primarily affects young infants: The median age of hospitalization was just 7 months, with 29.2% of admitted patients being neonates (0–2 months). RSV is a leading cause of hospitalization in infants under 6 months, with severity inversely correlating with age.
-HMPV targets older children and those with comorbidities: The median age of hospitalization was 16 months, with a greater impact on children over 1 year. Notably, the prevalence of underlying medical conditions (e.g., cardiovascular, neurological, respiratory) was more than twice as high in HMPV patients (26%) compared to RSV patients (11%), highlighting their heightened vulnerability.

Figure 1. Age distribution of ED visits and hospitalizations associated with RSV or HMPV
in children under 18.
Key Finding 2: Differentiating Clinical Presentations
-RSV manifests with prominent lower respiratory signs: It is strongly associated with bronchiolitis (76.7% of hospitalized cases). Key indicators include chest wall retractions (76.9% inpatients; 27.5% ED) and tachypnea (91.8% inpatients; 69.8% ED), both significantly more frequent than in HMPV.
-HMPV presents with higher fever and pneumonia risk: Pneumonia was diagnosed in 35.6% of hospitalized HMPV patients—double the rate of RSV. Fever was a more predominant feature (83.6% inpatients; 81% ED). While respiratory symptoms like wheezing and tachypnea occur, they are generally less severe than in RSV.
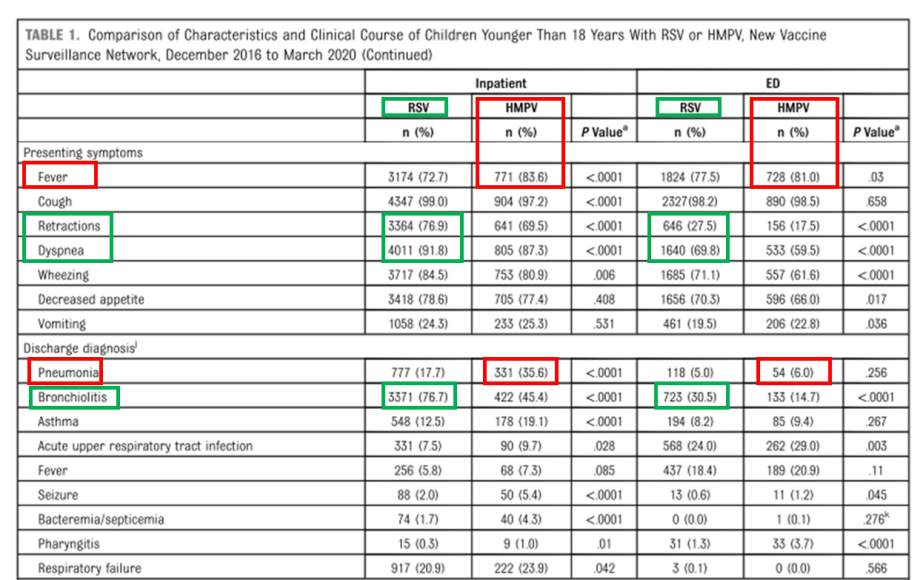
Figure 2. Comparative characteristics and clinical course of RSV vs. HMPV in children under 18.
Summary: RSV predominantly causes severe disease in younger infants, characterized by significant respiratory distress (wheezing, retractions) and bronchiolitis. HMPV more commonly affects older children with comorbidities, presents with pronounced fever, carries a higher risk of pneumonia, and often triggers a broader systemic inflammatory response.
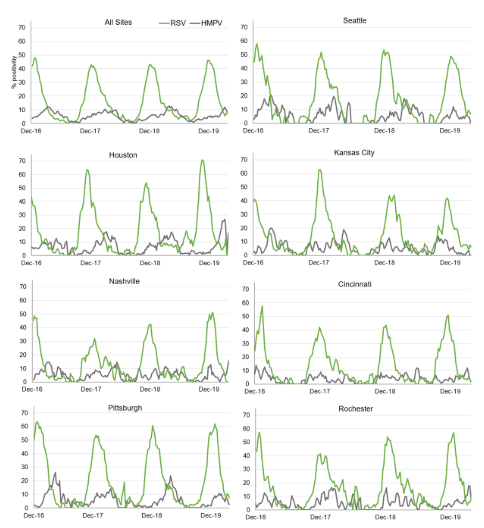
Key Finding 3: Seasonal Patterns Matter
-RSV has an early, predictable peak: Its activity is highly concentrated, typically peaking between November and January, making it the primary viral threat to infants in the autumn and winter.
-HMPV peaks later with greater variability: Its season arrives later, usually peaking in March and April, and demonstrates significant year-to-year and regional variation, often appearing as a “second wave” after RSV declines.
Figure 3. Overall and site-specific PCR positive rates for RSV and HMPV among children under 18 with acute respiratory infection (ARI)-associated ED visits and hospitalizations.
Prevention and Care: An Evidence-Based Action Plan
-RSV Prophylaxis: Prevention strategies are now available. In 2023, the U.S. FDA approved a long-acting monoclonal antibody (Nirsevimab), which can protect infants for their first 5 months. Additionally, maternal RSV vaccination effectively transfers protective antibodies to newborns.
-HMPV Prophylaxis: There are currently no approved preventive drugs. However, several vaccine candidates (e.g., AstraZeneca’s RSV/HMPV combination vaccine) are in clinical trials. Parents are advised to stay informed about updates from public health authorities.
Seek Immediate Medical Attention for ANY of These “Red Flags”:
-Fever in Infants: Temperature ≥38°C (100.4°F) in any infant under 3 months of age.
-Elevated Respiratory Rate: Breathing exceeds 60 breaths per minute for infants 1-5 months, or 40 breaths per minute for children 1-5 years, indicating potential respiratory distress.
-Low Oxygen Saturation: Oxygen saturation (SpO₂) falls below 90%, a critical sign of severe illness observed in 30% of RSV and 32.1% of HMPV hospitalized cases in the study.
-Lethargy or Feeding Difficulties: Notable lethargy or a reduction in milk intake by more than one-third within 24 hours, which can be a precursor to dehydration.
While distinct in epidemiology and clinical presentation, accurately differentiating between RSV and HMPV at the point of care remains challenging. Furthermore, the clinical threat extends beyond these two viruses, with pathogens such as influenza A and a spectrum of other viral and bacterial pathogens concurrently threatening population health. Timely and precise etiological diagnosis is therefore crucial for appropriate supportive management, effective isolation, and rational resource allocation
Introducing the AIO800 + 14-Pathogen Combined Detection Kit (Fluorescence PCR) (NMPA, CE, FDA, SFDA approved)
To meet this demand, the Eudemon™ AIO800 Fully Automatic Nucleic Acid Detection System, combined with a 14-pathogen respiratory panel, offers a transformative solution — delivering true “sample in, answer out” diagnostics in just 30 minutes.
This comprehensive respiratory test detects both viruses and bacteria from a single sample, enabling frontline healthcare providers to make confident, timely, and targeted treatment decisions.
Key System Features That Matter to Your Clients
Fully Automated Workflow
Less than 5 minutes hands-on time. No need for skilled molecular staff.
- Fast Results
Turnaround time of 30 minutes supports urgent clinical settings.
- 14 Pathogen Multiplex Detection
Simultaneous identification of:
Viruses:COVID-19,Influenza A & B,RSV,Adv,hMPV, Rhv,Parainfluenza types I-IV, HBoV,EV, CoV
Bacteria:MP,Cpn,SP
-Lyophilized Reagents Stable at Room Temperature (2–30°C)
Simplifies storage and transportation, eliminating cold-chain dependency.
Robust Contamination Prevention System
11-layer anti-contamination measures including UV sterilization, HEPA filtration, and closed-cartridge workflow, etc.
Rapid, comprehensive pathogen identification is foundational to modern management of pediatric respiratory infections. The AIO800 system, with its fully automated, 30-minute, multiplex PCR panel, provides a practical solution for frontline settings. By enabling early and accurate detection of RSV, HMPV, and other key pathogens, it empowers clinicians to make targeted treatment decisions, optimize antibiotic use, and implement effective infection control—ultimately improving patient care and healthcare efficiency.
#RSV #HMPV #Rapid #Identification #Respiratory #Pathogen #Sample-to-Answer #MacroMicroTest
Post time: Dec-02-2025