When a child develops a runny nose, cough, or fever, many parents instinctively think of the common cold or flu. Yet a significant share of these respiratory illnesses—especially the more severe ones—are caused by a lesser-known pathogen: Human Metapneumovirus (hMPV).
Since its discovery in 2001, hMPV has emerged as a major global contributor to respiratory infections, affecting not only children but also older adults and immunocompromised individuals.
Recognizing hMPV’s real impact is essential—not to heighten fear, but to strengthen awareness, improve clinical decision-making, and ultimately reduce the burden on healthcare systems and vulnerable populations.
The Underestimated Scale of hMPV
Although often buried within broad categories such as “viral respiratory infections,” the data reveal hMPV’s substantial public health significance:
A Leading Cause in Children:
In 2018 alone, hMPV was responsible for over 14 million acute lower respiratory infection and hundreds of thousands of hospitalizations in children under five.
Globally, it is consistently identified as the second most common viral cause of severe childhood pneumonia, after Respiratory Syncytial Virus (RSV).
A Significant Burden on Older Adults:
Adults aged 65 and older face a high risk of hospitalization due to hMPV, frequently presenting with pneumonia and severe respiratory distress. Seasonal peaks—typically in late winter and spring—can place additional strain on healthcare services.
The Challenge of Co-infections:
Because hMPV often circulates alongside influenza, RSV, and SARS-CoV-2, co-infections occur and can lead to more severe illness while complicating diagnosis and treatment.
Why hMPV Is More Than “Just a Cold”
For many healthy adults, hMPV may resemble a mild cold. But the virus’s true severity lies in its propensity to infect the lower respiratory tract and its impact on specific high-risk groups.
A Broad Spectrum of Illness
hMPV can cause: Bronchiolitis; Pneumonia; Acute exacerbations of asthma; Worsening of chronic obstructive pulmonary disease (COPD)
Populations at Greatest Risk
-Infants and Young Children:
Their smaller airways are highly vulnerable to inflammation and mucus accumulation.
-Older Adults:
Declining immunity and chronic diseases increase susceptibility to severe complications.
-Immunocompromised Patients:
These individuals may experience prolonged, severe, or recurrent infections.
The Core Challenge: A Diagnostic Gap
The main reason hMPV remains under-recognized is the lack of routine, virus-specific testing in many clinical settings. Its symptoms are nearly indistinguishable from other respiratory viruses, leading to:
-Missed or Delayed Diagnoses
Many cases are simply labeled as “viral infection.”
-Inappropriate Management
This may include unnecessary antibiotic prescriptions and missed opportunities for proper supportive care or infection control.
-Underestimation of True Disease Burden
Without accurate diagnostic data, hMPV’s impact remains largely hidden in public health statistics.
RT-PCR remains the gold-standard for detection, highlighting the need for more accessible and integrated molecular testing solutions.
Closing the Gap: Turning Awareness into Action
Improving hMPV outcomes requires both greater clinical awareness and access to rapid, accurate diagnostics.
1. Strengthening Clinical Suspicion
Healthcare providers should consider hMPV when evaluating patients—especially young children, older adults, and immunocompromised individuals—during peak respiratory seasons.
2. Strategic Diagnostic Testing
Implementing rapid, multiplex molecular testing enables:
Targeted Patient Care
Proper supportive treatment and reduction of unnecessary antibiotic use.
Effective Infection Control
Timely cohorting and isolation to prevent hospital outbreaks.
Enhanced Surveillance
A clearer understanding of circulating respiratory pathogens, supporting public health preparedness.
3. Innovative Diagnostic Solutions
Technologies such as the AIO800 Fully Automated Nucleic Acid Detection System directly address current gaps.
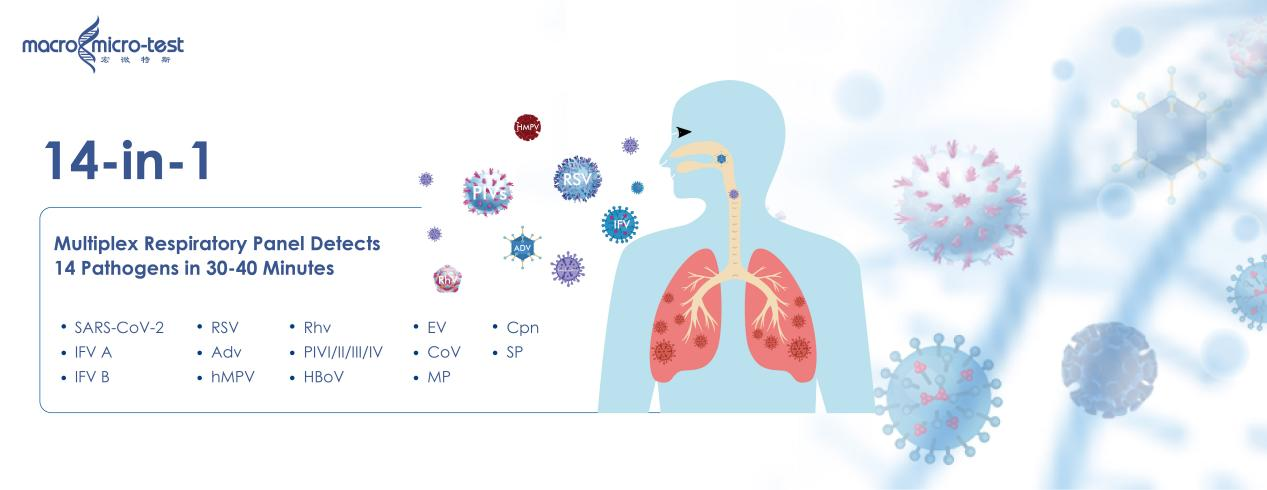
This “sample-in, answer-out” platform detects hMPV alongside 13 other common respiratory pathogens—including influenza viruses, RSV, and SARS-CoV-2—within approximately 30 minutes.
Fully Automated Workflow
Less than 5 minutes hands-on time. No need for skilled molecular staff.
- Fast Results
Turnaround time of 30 minutes supports urgent clinical settings.
- 14 Pathogen Multiplex Detection
Simultaneous identification of:
Viruses:COVID-19,Influenza A & B,RSV,Adv,hMPV, Rhv,Parainfluenza types I-IV, HBoV,EV, CoV
Bacteria:MP,Cpn,SP
-Lyophilized Reagents Stable at Room Temperature (2–30°C)
Simplifies storage and transportation, eliminating cold-chain dependency.
Robust Contamination Prevention System
11-layer anti-contamination measures including UV sterilization, HEPA filtration, and closed-cartridge workflow, etc.
Adaptable Across Settings
Ideal for hospital labs, emergency departments, CDCs, mobile clinics, and field operations.
Such solutions empower clinicians with rapid, reliable results that can guide timely and informed decisions.
hMPV is a common pathogen with an uncommonly overlooked impact. Understanding that hMPV goes “beyond the common cold” is critical for improving respiratory health outcomes.
By combining greater clinical vigilance with advanced diagnostic tools, healthcare systems can more accurately identify hMPV, optimize patient care, and reduce its significant burden across all age groups.
Post time: Dec-08-2025
